ABOUT HIPS & KNEES


Dr Michael McDonald – Orthopaedic Surgeon
Dr Michael Charles Edward McDonald, is a healthcare practitioner, specialising as an Orthopaedic Surgeon, in Bryanston, Sandton, Gauteng.
He completed his MBChB at the University of Pretoria where he attained his MMed (Orth) and has been working at Medi-Clinic Sandton since 2007 in collaboration with Professor Frans Weber. He was involved in surgery in the teaching of young Orthopaedic surgeons in primary and revision Hip and Knee surgery.
His passion for special interest lies in Total Hip and Knee Replacements and in particular minimal invasive and tissue sparing surgery – the Anterior Approach.
Dr McDonald attended local and international instruction in minimally invasive surgery. This is a revolutionary approach where no muscles are cut, patients have less pain and mobilize much quicker. It also allows for accurate leg length determination. Dr McDonald chooses the best approach for each patient and prefers the Rottinger approach, the newest technique in MIS Hip surgery as he was taught by Dr Bringer of France.
Dr McDonald’s practice is well established and his highly professional team will guide and assist patients from getting quotations, authorization, and also through surgery and recovery to full rehabilitation.
Dr Mc Donald cares for a variety of hip and knee problems, including joints that have been damaged by arthritis and injuries.
MY HOSPITAL STAY
Time of admission to hospital is 12 noon to 1pm on the day before surgery. We prefer patients to be admitted the day before, to meet the Physiotherapist for preparation for the post-operative phase, and to do final evaluation and tests if needed. We rather allow patients out of hospital earlier, not pushing up the total cost of hospitalization.
Same day admission is becoming popular and cost effective. Certain medical aids do not allow admission the day before. And then the pre-operative regime is adjusted accordingly.
The team will visit you on the morning of surgery. Please be advised that everything will be done to keep your position on the list but sometimes you might need to be moved as preference is given to frail and sick patients.
The operation takes about 75 minutes.
When you wake up in recovery and the anaesthetist is satisfied with your progress you will be moved to high care.
When you recover from the anaesthetic you will be in a high care unit overnight. There will be a dressing on your thigh and drainage tubes from the wound into suction bellows. There will also be a tube into veins of your arm to be used to administer bloods, fluids, antibiotics and pain killers. Intravenous tubes are usually removed 24 hours after surgery, and the drainage tubes from the wound are usually taken out the second day after the operation.
WALKING
You will be using two crutches (elbow) or a walking frame when you get up to o walk for the first time. By the time you leave the hospital you should be walking comfortably and climbing one set of steps. Crutches must be discarded only after four weeks and after your follow-up visit to the surgeon (this is for primary surgery only).
Skin clips are removed 14 days after surgery. The wound should be healed by now, and if the physiotherapist is satisfied with your progress (walking and performing all the other exercises you are given to you).
You may not drive a car on discharge day after the operation and you must sit in the front seat if you are a passenger.
You must see the surgeon 6 weeks and again 6 months after the operation. If you live far from Johannesburg, you can arrange to have X-rays sent at these times. It is only between 6 and 12 months that you can expect to have reached the final, or near final result of your replacement operation. This period could be much longer in the case of revision surgery. Routine follow up visits 3, 5 and 10 years etc.
For the first few months after the operation you may experience swelling of the operated leg (usually down in the mornings, up in die evenings).
After having been discharged you will be required to take anti-coagulation medication Predaxa or Xeralta for four weeks (unless there is a contra indication, such as peptic ulcers). You will be given precise instructions before you leave the hospital.
Should you experience any pain in your chest or calf after discharge, report this to your doctor without delay. The risk of blood clots remains until about 8 weeks afterwards.
You should ask your dentist or general practitioner to prescribe a course of antibiotics if any major dental work has to be done, or if you have any infection anywhere else in your body. Germs spread via your blood stream and can affect the prosthesis: this should be avoided at all costs. At the 6 week follow up visit, a card with instruction will be supplied. The American Dental Association regards as a very low risk that of hip infection caused by dental work in healthy, active individuals. For the rest antibiotics prophylaxis is mandatory.
You will receive a take home medication (blood thinners and analgesics). There will be a follow up appointment date for your 6 week check up. Please do not shower for at least 10 days after the operation. Continue with walking aids and the exercises advised by your physiotherapist. After 6 weeks you can return to a normal life but total recovery time can take up to 1 year.
WHEN CAN I START TO DRIVE?
Patients with left knee replacements can drive an automatic car after 3 weeks.
Patients with right knee replacements can only drive after 6 weeks.
REFERENCES
- Which Implant Should We Use for PrimaryTotal Hip Replacement?
A Systematic Review and Meta-Analysis J. Christiaan Keurentjes, MD, Bart G. Pijls, MD, PhD, Floris R. Van Tol, MSc, Jill F. Mentink, MD. - Fatal pulmonary embolism following elective total hip arthroplasty: a 12-year study.
Bayley E1, Brown S2, Bhamber NS3, Howard PW4. Bone Joint J. 2016 May;
98-B(5):585-8. doi: 10.1302/0301-620X.98B5.34996. - Antibiotic Prophylaxis for Patients after Total Joint Replacement.
Information Statement from the American Academy of Orthopaedic Surgeons. - Crosslinking experience in South Africa. A du Plessis, C.J. Grobbelaar, F.A. Weber.
www.gammalink.co.za
Dr Mc Donald cares for a variety of hip and knee problems, including joints that have been damaged by arthritis and injuries.
REHABILITATION AFTER SURGERY
The following arrangements should be made by you prior to being admitted for surgery. For approximately 4-6 weeks after being discharged, as you will be unable to live alone or be on your own.
- Step-down facility
You need an authorization number from your medical aid to pay for the step down facility prior to admission for surgery. Your medical aid might request a motivational letter from your doctor, please contact the rooms and arrange with the secretary to fax a letter to the medical aid. - Home Care
You need 24 hours assistance at home if you don’t have a family member or domestic help. You need to contact your medical aid and ensure whether they will pay for home nursing. - Double story homes
If you have a staircase and are unable to stay on the ground floor, you need to make arrangements with your medical aid to pay for an ambulance to assist you prior to admission. Also make sure which ambulance service provider your medical aid uses. - Bath/Shower
You cannot bath for the first 6 weeks, you need to shower and therefore need assistance.
Prophylactic antibiotic cover for certain dental procedures is now only routinely given the first two years post operatively in healthy patients and routinely post operatively in immuno-compromised patients e.g. inflammatory, arthroplasty such as rheumatoid arthritis, malignancies, cortisone treatment etc. A single pre-operative dose of anti-biotic is advocated.
Spilling of bacteria into the bloodstream is called bacteraemia, and the bigger the dental procedure, the bigger the spill. (3) It should be noted however that chewing, tooth brushing and dental flossing lead to bacteria in the bloodstream 50% of the time. Normally however the body defences clears it up in the about 10 minutes.
SUGGESTED ANTIBIOTIC PROPHYLAXIS REGIMES
| PATIENT TYPE | SUGGESTED DRUG | REGIME |
|---|---|---|
| NOT ALLERGIC TO Penicillin Amoxicillin |
Cephalezin Cephradine |
2grams orally 1 hour prior to Dental procedure |
| ALLERGIC TO Penicillin Amoxicillin |
Clindamycin | 600mg orally 1 hour prior to Dental procedure |
There is evidence that 2g is equivalent to 3g oral amoxicillin with less risk of nausea.
No second doses are recommended for any of these dosing regimens.
| PROCEDURE | ANTIMICROBIAL AGENT | DOSE | TIMING | DURATION |
|---|---|---|---|---|
| Dental |
Cephalexin, cephradine, amoxicillin |
2 gm PO |
1 hour prior to procedure |
Discontinued within 24 hours of the procedure. For most outpatient/office-based procedures a single pre- procedure dose is sufficient. |
| Ophthalmic |
Gentamicin, tobramycin, ciprofloxacin, gatifloxacin, levofloxacin, moxifloxacin, ofloxacin, or meomycin- gramicidin-polymyxin B cefazolin |
Multiple drops topically over 2 to 24 hours or 100 mg subconjunctivally |
Consult ophthalmologist or pharmacist for dosing regimen |
|
| Orthopaedic |
Cefazolin Cefuroxime OR Vancomycin |
1-2 gIV |
Begin dose 60 minutes prior to procedure |
|
| Vascular |
Cefazolin OR Vancomyin |
1-2 g IV |
Begin dose 60 minutes prior to procedure | |
| Gastrointestinal | ||||
| Esophageal, gastroduodenal |
Cefazolin |
1-2 gIV |
Begin dose 60 minutes prior to procedure | |
| Biliary tract |
Cefazolin |
1-2 gIV |
Dependent on time of procedure, consult with GI physician and/or pharmacist |
|
| Colorectal |
Neomycin + erythromycin base (oral) OR metronidazole (oral) |
1 gIV |
Dependent on time of procedure, consult with GI physician and/or pharmacist |
|
| Head and neck |
Clindamycin + gentamicin OR cefazolin |
600-900 mg IV |
Begin dose 60 minutes prior to procedure | |
| Obstetric and gynaecological |
Cefoxitin, cefazolin Ampicillin/sulbactam |
1-2 gIV |
Begin dose 60 minutes prior to procedure | |
| Genitourinary |
Ciprofloxacin |
500 mg PO or 400 mg IV |
Begin dose 60 minutes prior to procedure |
Your Physiotherapist will show you how to manage many daily functions that will prevent damaging your new hip.
RULES FOR THE BEST RESULTS
Never take your operated leg across the midline – for the first 3 months.
To shower is best. But beware…. don’t shower until the wound is completely healed or sealed, approximately 5 days after clips removed.
Crutches and your feet can slip easily when wet. Be careful.
HOW TO GET OUT OF BED
Move to the side of the bed nearest to the operated leg. Let operated leg bend, keeping thigh on the bed.
Then sit up, and continue turning until your knee is on the outside of the hip, which can be done by moving to the bottom of the bed.
THE CORRECT SITTING POSTURE
Objects on the table must be near enough to reach without bending forward and thus taking your back off the backrest.
The moment you take your back off the backrest of the chair you will be bending more than 90 degrees. With good muscles and minimally invasive techniques (Anterior approach), these rules can be bent on consent of your surgeon.
SITTING IN A WHEELCHAIR
Your knee will be higher than your hip if you bend your knee to put your feet on the footrest. Keep your leg straight to the front and use a pillow to pad the footrest.
CLIMBING STEPS
- Going up
Step up with your good leg, followed by operated leg and finally your crutches. - Going Down
Crutches first, operated leg next while bending your good leg to lower yourself. Finally put your good leg down.
WALKING
Take crutches forward, then the operated leg so that toes are more or less in line with the crutches. Tighten your knee firmly while the good leg goes beyond the crutches. Paces should be kept at the same size.
TO PICK SOMETHING UP FROM THE FLOOR
The best way is to call someone else to do it for you.
If necessary (for example if you have dropped your crutch) bend towards the good side keeping foot of operated leg on the floor.
SOME FINAL COMMENTS
- You will only be allowed to drive a car after 6-8 weeks. It is better to avoid travelling before this unless it is absolutely necessary.
- You will be required to stay 2 weeks on 2 crutches and thereafter on one crutch or stick in the hand opposite to surgery for another 2 weeks.
- For younger people and those with good muscles this period of assisted weight bearing could be reduced, and in patients with complex surgery and bone grafting procedure period of persisting weight bearing could lengthened.
- Sexual intercourse is permitted from 4 weeks onwards.
- Post-operative activities: The patient should not indulge in running, jumping or contact sports. Confine activity to walking, swimming and cycling in moderation. An artificial hip is expected to last at least 15 years and although designs and materials are constantly improving, poor quality bone and the different mechanical characteristics from bone and prosthesis remain a major cause of failure of prosthesis. Jumping and running can for example place a load of 30 times body weight on the prosthesis and the ceramic ball could break.
- It is important for post-menopausal women to have at least one bone density scan either before or after surgery to monitor possible osteoporosis. Plain X-rays only demonstrate osteoporosis after 30 – 50% of bone has been lost.
- Hip Surgery technology is updated all the time, as well as rehabilitation thereof. We should however remember that the human body has not been updated for at least 250 000 years, thus the basic healing process remains the same, and we only facilitate the process.
Dr Mc Donald cares for a variety of hip and knee problems, including joints that have been damaged by arthritis and injuries.
FAQs FREQUENTLY ASKED QUESTIONS
WHY DO HIP JOINTS FAIL?
IS THE OPERATION REALLY NECESSARY?
HOW LONG WILL A REPLACEMENT LAST?
WHAT HAPPENS IF THE OPERATION IS A FAILURE? CAN IT BE RE- DONE?
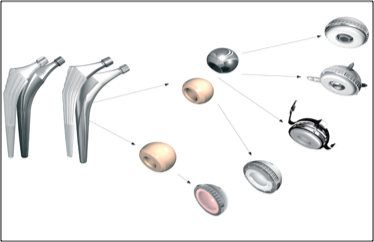
WHICH MATERIALS ARE USED?
WHICH TECHNIQUE IS BEST?
CAN BOTH HIPS BE DONE SIMULTANEOUSLY?
WHAT ARE THE RISKS IN REGARD TO ANAESTHESIA (both general and spinal)?
WILL I NEED A BLOOD TRANSFUSION?
HOW LONG WILL MY HOSPITAL STAY BE?
WHAT ARE THE POSSIBLE COMPLICATIONS?
HOW CAN I HELP TO MAKE SURGERY A SUCCESS?
WHY DO HIP JOINTS FAIL?
There are many causes of osteoarthritis of the hip joint but in all cases the gliding action of the cartilage upon itself fails, the surface roughens up. This can be caused by age related deteriosation, infections, injuries, overuse of joints, poorly fitting head in socket (congenital dysplasia), avascular necrosis, Perthe’s disease, and many other causes. The eventual outcome is poor movement of the hip joint with the cartilage worn away not unlike the tread of a tyre being worn away.
When other non-surgical and in some case surgical treatments of the arthritic hip have failed, total joint replacement is often the only way out. This is a procedure whereby the ball and socket of the hip joint are replaced by an artificial ball and socket.
IS THE OPERATION REALLY NECESSARY?
This is the most difficult decision of all, for the surgeon as well as the patient.
Factors that influence the decision are:
- Pain
- Loss of function (the patient’s movements are severely curtailed, walking becomes a problem, as well as bending down to put on shoes or wash feet etc.)
- Changes that occur in X-rays taken over a period of time.
- Poor response to anti-inflammatories, especially the occurrence of side effects.
Patient
Here the decision will depend on pain and on loss of function. If his/her condition affects quality of life and/or working ability, the patient must decide whether this condition is serious enough to warrant the operation, almost regardless of age.
Surgeon
The surgeon takes all these above factors into account, in addition to other factors such as age and pathology, before advising the paient. By and large we are more lax with these indications above age 60, and stricter in younger patients.
HOW LONG WILL A REPLACEMENT LAST?
There are adequate methods of uncemented as well as cemented fixation to the skeleton, but as hip replacements last longer and longer the main problems, especially in younger people are component wear (a problem virtually solved), secondary loosening, and bone destruction. Often the interface between prosthesis and bone can get damaged by wear particles. The tendency is towards uncemented fixation of prosthesis even allowing for playing of limited sport where the bone quality is adequate.
There is the danger that an implant can fail at any time if, for example, there is an unexpected loosening caused by an infection, or by collapse of the bone, in which case it cannot support the prosthesis. This is why sporting activities, for example, should be limited and discussed in detail with the surgeon. In general if the patient is too active, it can lead to early failure of the hip replacement.
Follow up studies of large series of these procedures show that at least 90% of the hip replacements performed still function after 10 years (i.e. 1% failure rate per year). Recently, the National Institute for Health and Care Excellence (NICE) suggested a ten-year revision rate of 10% as an acceptable benchmark performance of a primary total hip implant, which was loosely based on an earlier report by Murray et al.
Among patients over age 65 the failure rate is lower and in younger and more active groups it can be as much as five times higher. On average the aim is to have at least 90% 15 year survival of the hip implants. Many 25 and 30 year total hip survivals are commonly seen in arthroplasty practice worldwide. And with crosslinking methods developed in South Africa 35-38 year follow of survivors is in progress, with wear a low as 0.018mm/year.
WHAT HAPPENS IF THE OPERATION IS A FAILURE? CAN IT BE REDONE?
If there is enough bone, the operation can be re-done. During initial surgery the surgeon is constantly aware of bone preservation, a most important consideration in the procedure.
Patients must also be aware of bone preservation and look after the prosthesis by following instructions to the letter.
When and if the prosthesis shows signs of failure, like limping and shortening, consult your surgeon immediately. Delay in having a revision operation performed when loosening occurs causes bone destruction. Remember, pain is not always a feature of loosening.
WHICH MATERIALS ARE USED?
High density Polyethylene, Ceramic, Stainless Steel, Chrome Cobalt and Titanium Alloys are most commonly used in specific engineering combinations to ensure low friction, low wear and low fatigue. Cemented and uncemented prosthesis are available. Significant Biomaterial refinements take place all the time.
The Highly Crosslinked Ultra High Molecular Weight Polyethylene (UHMWPE), is infinitely stronger and more wear resistant, and less bone damage now occur from wear particles. Wear can be as little as 0,018 mm per year.
The ceramics that have been plagued by either fractures or phase transformation roughening up smooth surfaces and actually increasing wear in certain instances, have been much improved and combination of certain ceramics like alumina and zirconia have virtually taken away the risk of component fracture, with minimal wear.
The ASR prosthesis: in a recent communication from the British Orthopaedic Association warned that 49% failure can occur in 6 years.
The tendency is towards uncemented fixation of prosthesis even allowing for playing of limited sport where bone quality is adequate. The prosthesis is covered with plasma sprayed hydroxyapatite to facilitate firm bonding to bone.
Cemented fixtion is used to fixate a highly polished stem or a polyethylene cup to the bone. A combination which is very popular and has a good outcome is called a hybrid, this is a cemented stem and an uncemented cup. This latter method is preferred for over 65 year old, especially in osteoporotic bone.
Commercially available prostheses are subject to extremely stringent design and manufacturing requirements. Some prostheses do well in some patients, others are more suitable for others, depending on the specific disease or on other factors like age and activity. This is a decision that has to be made by the surgeon who will have all the necessary information at his disposal and will endeavour to make the best decision in each case.
WHICH TECHNIQUE IS BEST?
Lateral/Hardinge approach:
This is the surgical approach that is used from the side, you will have an incision that can 10 -30cm on your skin. The length is determined by the surgeon’s need to visualise your hip socket. For primary surgery it is usually a smaller incision. The muscles(abductor) that help move your hip joint are split and very carefully reattached. Sometimes you can develop a limp because of weakening of these muscles.
Posterior approach:
For the Posterior approach you will have an incision of similar length 10-30cm depending on the degree of difficulty of the surgery. The hip abductors (muscles) are not cut during this approach. There is a slightly higher risk of dislocation with this approach.
Anterior approach:
This is the most modern and there are different versions, Dr McDonald uses the Rottinger approach. You will have a 10-15 cm incision on the front part of your leg. With the Rottinger approach there is less chance of nerve damage and minimal damage is done to the muscles because of less retraction, there is NO cutting of the muscles. Patients tend to mobilise very soon after surgery and this approach has seen hospital stays decrease significantly. Patient selection is very important. Ask your surgeon if you qualify for this approach. This approach has less risk of anterior dislocation, and virtually no swelling necessitating ice packs. The surgery takes place below rather than above the tensor fascia lata, muscle no traction table is necessary that could tilt the pelvis and compromise positioning.
CAN BOTH HIPS BE DONE SIMULTANEOUSLY?
The answer is yes, but it is a major procedure and places an enormous responsibility on the surgeon, the anaesthetist and the staff involved in post-operative care. This is done only in exceptional cases: if both hips need to be replaced, it is better to have them done separately, allowing about six months between operations. The Rottinger approach has made this procedure more practical by reducing morbidity, operating time and recovery.
WHAT ARE THE RISKS IN REGARD TO ANAESTHESIA (both general and spinal)?
In the hands of an expert, the risk factor is very low, especially as all potential problems are evaluated and necessary precautions taken before the operation takes place. A consultation pre-operatively with a specialist physician and anaesthetist is very important especially in older patients and those with medical problems. Both general and spinal or epidural type anaesthesia is acceptable and is done with a high success rate.
WILL I NEED A BLOOD TRANSFUSION?
Due to improved technology, presently very few patients require blood transfusions for primary surgery or the less complicated revision surgery.
PLEASE DISCUSS WITH YOUR SURGEON.
HOW LONG WILL MY HOSPITAL STAY BE?
A patient could be ready to go home on day 2, 3-5, if domestic circumstances and an adequate back up system does not exist at home or in a “step down” facility, it is better to stay longer.
Likewise the surgeon and team should be careful not to push the envelope of quick recovery too far. The smaller incision and fast tracking only provides an advantage for the first 6 weeks and no advantage at 6 months over other techniques.
Remember, we are dealing with a 30 year investment.
WHAT ARE THE POSSIBLE COMPLICATIONS?
1. Infections
Infections of the chest and urinary tract of the operated area (in this case the hip) can occur. Such infections can be deep or superficial. In the event of a deep infection in the operated area, the prosthesis has to be removed and the operation re-done. Fortunately, this does not occur often, but if it does the management is very costly and not always successful. Deep infections of the hip can occur years after surgery and is usually blood borne – it is however very rare.
Our published incidence of deep infection in Sandton Clinic over 4 166 cases was 0.5%, decidedly better than the 1 – 2% accepted incidence in the scientific literature.
2. Dislocation
This occurs when the prosthesis comes out of the socket. In uncomplicated surgery this does not often happen, but patients must be aware of the possibility, especially during the first six weeks, so that they do not become casual about the very specific instructions they are given on how to move and how not to move. See attached diagrams. It is more common after revision surgery. Closed reduction is usually possible. Here surgical technique is of the utmost importance, as component orientation and the tissue tension are dependent on surgical technique.
Late dislocations can occur when there is wear on the implant and lax tissues, especially with prostheses with smaller heads.
Revision surgery is the treatment of choice.
3. Blood clotting
Deep venous thrombosis (DVT).
According to statistics for hip surgery, there is a 50% – 60% chance of blood clots occurring in the calf or lungs if no blood thinning prophylaxis is administered. These can migrate to the lungs as clots or pulmonary emboli. Doctors are fully aware of this and have an established procedure to deal with the problems. With proper blood thinning methods and close post-operative supervision (which includes an X-ray control, called a Venogram, of the operated limb, or a Doppler or Nuclear isotope study), clots can be diagnosed early. The incidence of blood clotting is now reduced and if any complications of this kind do occur, they can be dealt with immediately and more effectively than in cases where the precautions are not taken. The incidence of a life threatening clot is low.Early mobilisation reduces these risks.
4. Other complications
- Other complications documented in the literature – fortunately seen very rarely.
- Damage to surrounding blood vessels and nerves.
- Fracture of bone surrounding the implant
- Diminished range of motion of the joint
- Swelling of the leg: Lie down with the swollen leg elevated on enough pillows so that the heel is higher than the chest wall. “Pump” the foot up and down.
- “Allergy” to the prosthesis
- Persistent joint pain
- Leg length discrepancy
- Component fracture especially ceramic balls that can break. The incidence is presently predicted at 1:10 000 (ten thousand).
- Prophylactic measures taken routinely should prevent most infections.
HOW CAN I HELP TO MAKE SURGERY A SUCCESS?
Do not withhold any medical information about yourself, no matter how insignificant it may seem to you. You must list all medication you take and give this list to the surgeon: for example, if you are taking cortisone, medication for blood pressure, oral contraceptives, anti-inflammatory tablets or salicylates. Hormone replacement therapy, salicylates, anti-inflammatories and anti-coagulants should be stopped altogether about one week before surgery. This will reduce the risk of bleeding.
A pre-operative medical evaluation is essential. Please bring the reports on blood and other tests done by your physician or local doctor and give them to the ward sister.
See your dentist both before and after the operation to make sure that there are no dental infections of any kind. Also inform your general practitioner before and after the operation in the event of any suspicion of infection.
Lose weight if you are overweight. This will dramatically decrease the risks associated with a hip replacement procedure. One of the reasons of post-operative limping is the difficulty of doing surgery through very big thighs, resulting in muscle damage.
Stop smoking.
Try to improve your general health before surgery: the fitter you are the better.
Fill out the questionnaire on anaesthetics attached to this brochure.
Alcohol after the operation: a “night cap” in the ward is allowed if you are used to it, but please bring your own liquor.
CONTACT DR MICHAEL MC DONALD
Mediclinic Sandton,
Main Road,
Bryanston,
Sandton,
Johannesburg
Phone: 011-7061244
Fax: 011-706 2301
Email: mcemac@mweb.co.za
Reception: vicky@hipsandknees.co.za